Ever wished you could be more in control of when you have your period – or even skip it for a few months altogether?
Whether you want to enjoy that big event or holiday (think swimming or wearing white trousers without worrying), or you’d like a break from periods for your health or sex life, it can be handy to be able to avoid your period. Not to mention those other issues you might get with your monthly bleed, from pain to PMS.
There’s no natural way to delay your period, but there are medicines that may do the trick, including period-delay medication such as norethisterone and hormonal contraception such as the pill.
So here’s what you need to know about how to delay your period – both as a one-off or longer term – including the possible benefits, what medicines are available, and how they might work for you.
What are the benefits of skipping or delaying a period?
It can be empowering to know that you can take control of your periods. In some cases, that may be because you have an unpredictable cycle or troublesome period symptoms, which can leave you feeling frustrated to be at the mercy of your body.
In other cases, it can simply be good to know you don’t have to work out if your period is going to clash with your best friend’s wedding, or that family beach holiday.
You’re also unlikely to miss the bother and expense of buying period products such as pads or tampons, and remembering to change your period protection frequently.
How skipping a period can be good for you
Skipping periods can not only make you feel more in control, but can also help with period-related problems. Symptoms or conditions that skipping periods can help with include:
- heavy periods – excessive blood loss every month can take its toll physically and emotionally, and can also lead to iron deficiency anaemia, which can leave you feeling very tired (fatigued), but skipping periods can help avoid this. Read about other solutions in our heavy periods survival guide
- painful periods – if your periods cause cramping tummy pains or lower back ache, skipping a period can give you a well-needed break. Read more about period pain and the best ways to stop it
- irregular periods – not knowing when your period is coming can be annoying, but delaying or skipping it can put you back in control. Read more about treatment for irregular periods
- premenstrual syndrome (PMS) – PMS symptoms you can get before your period range from bloating and mood swings to acne and breast pain, but not having a ‘natural’ cycle can reduce your chances of getting them. Learn more in our ultimate guide to PMS
- endometriosis – this long-term (chronic) condition can cause heavy and painful periods, but hormonal treatments that stop your periods can help ease symptoms. Read more about endometriosis treatment
- fibroids – these non-cancerous growths that can develop in or around your womb can also cause heavy or painful periods, so skipping or stopping periods can help manage symptoms. Read more about fibroids treatment
- blood clotting disorders – conditions that cause bleeding, such as Von Willebrand disease, often cause heavy periods, so not having periods can make symptoms easier to manage
- other health conditions – several other health conditions can be aggravated or made worse by having periods, including migraines, asthma and irritable bowel syndrome (IBS)

Is it ‘healthy’ to skip a period?
Despite what you might think, periods aren’t essential for your health. Unless you’re trying to get pregnant, you don’t need to release an egg (ovulate) and have periods. And if you choose to use a hormonal method to skip a period, you won’t store up extra blood or cause other health risks.
The idea that monthly periods are ‘healthy’ is partly down to the way the combined contraceptive pill was designed – so that you stop taking the pill for 7 days each month to have an artificial period. But these ‘withdrawal bleeds’ have no medical benefits, and it’s safe to take the pill continuously or ‘back to back’ (see below.
If you have any concerns about taking hormonal contraception in the long term, your doctor can advise on the most appropriate method for you.
However, if you’re regularly skipping or missing periods and you're not using hormonal contraception, speak to your doctor, as you may have an underlying condition that needs treatment. Read more about absent or missed periods.
How to delay your period
If you’re not taking the combined pill and you want to delay your period, talk to your doctor or pharmacist about the following options.
Norethisterone
Sometimes known as the ‘holiday hormone’, norethisterone can be prescribed by your doctor or some online pharmacy services. Here’s what you need to know:
- you can take it to delay your period for up to 17 days
- you’ll usually start taking it about 3 days before your period is due, and your period should start 2 to 3 days after you stop
- it isn’t suitable for everyone, including if you’re at higher risk of blood clots or breast cancer
- many women use it to delay their periods when they’re going on holiday – but how well it works varies from person to person
- when used in the longer term to treat period-related conditions, 1 small study found blood flow was reduced by 87% by the end of 3 months of taking it – but no participants said their periods stopped completely
- 1 small study of women with endometriosis found 94% had no periods after taking it daily for 6 months
Medroxyprogesterone acetate
Medroxyprogesterone acetate can be prescribed ‘off-label’ to delay periods (which means it can be prescribed to do something other than what it’s licensed for). You can also buy it from a pharmacy. Here’s what you need to know:
- it contains an artificial form of the hormone progesterone
- it can delay your period for up to 17 days
- as with norethisterone, you take it from a few days before your period is due
- it has a lower risk of blood clots than norethisterone
- it’s increasingly being used to delay periods because it’s a safer alternative to norethisterone
- some evidence suggests it might not be as effective as norethisterone, but more research is needed
How to skip your periods
There are a few different ways you can avoid having a period altogether, which can be used either short or longer-term. Most options are forms of hormonal contraception. You should talk to your doctor about what might be suitable for you.
The combined pill
The combined contraceptive pill contains the hormones oestrogen and progesterone, and you can take 2 or more packets ‘back to back’ without a break to avoid having a period. Talk to your doctor at your next pill check for more information, and to check your pill can safely be taken in this way.
Whether – and how – you can do this will depend on the type of combined pill you’re taking:
- monophasic pills – you usually take these pills every day for 21 days, then have a 7-day gap, when you have a period. But if you want to skip your period, you start a new packet of pills straight away, without leaving a gap
- everyday pills – the first 21 pills in a pack contain active ingredients that stop you becoming pregnant, while the remaining 7 days are dummy pills. You usually have a period while you take the last 7 tablets. But if you want to skip a period, you miss the last 7 pills in the pack and start your new packet straight away
- phasic 21 day pills – these can’t be taken back to back, as they contain different combinations of hormones and you need to take them in the right order to prevent pregnancy
What you need to know about taking the pill back to back:
- you won’t usually won’t get a period – about 20% of people get irregular bleeding when they first start using the combined pill, but this usually settles down
- you can take it continuously in the long term (as long as your doctor says it’s safe for you) if you don’t want to have periods
- you may get some spotting or what’s known as ‘breakthrough bleeding’ in the first few months of continuous pill use (and also occasionally later on) – but this usually becomes spaced out and stops over time
What to do if you bleed while taking the pill back to back:
- if you have bleeding for 4 continuous days, stop taking the pills for 4 days (remove the pills you’re skipping from the packet and dispose of them safely)
- during those 4 pill-free days, you’ll continue to bleed – and you’re still protected from pregnancy
- on the 5th day, start taking your pills again, and continue to take the packets back to back
- if you regularly get bleeding or spotting, speak to your doctor, as you may need a different pill

The progestogen-only-pill (POP, mini pill)
Also known as the mini pill, the progestogen-only pill just contains progesterone. Here’s what you need to know:
- unlike the combined pill, it’s designed to be taken every day, with no break between packs
- it can make your periods lighter or stop them altogether – though it can also make them more frequent or irregular
- after a year of use, about 50% of women will have no periods or infrequent bleeding
The vaginal ring
The vaginal ring is a small contraceptive device that fits inside your vagina and releases low doses of oestrogen and progesterone. Here’s what you need to know:
- you usually take it out after 21 days and have a 7-day gap before replacing it – but if you want to skip your period, you can put a new ring in straight away
- as with the combined pill, you can use it back to back continuously to avoid having periods in the longer term
- it’s effective at stopping periods, but you may get some spotting or breakthrough bleeding for the first few months of using it continuously
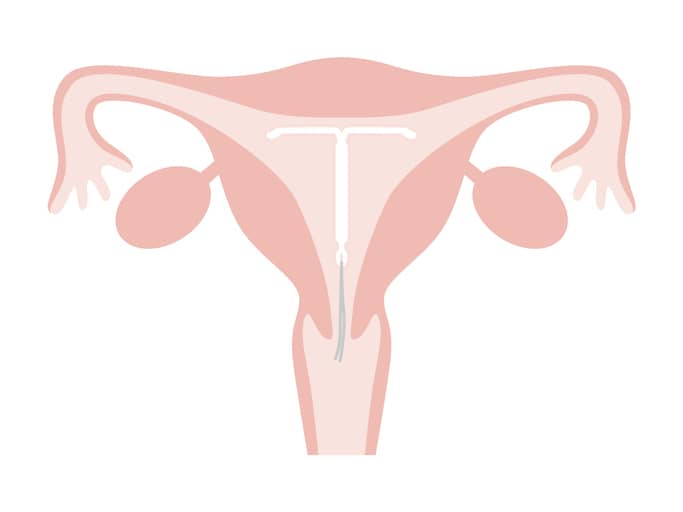
The intrauterine system (IUS)
An intrauterine system (IUS) is a small contraceptive device that fits inside your womb and releases progesterone. Here’s what you need to know:
- it’s a long-lasting method of contraception – once it’s fitted and in place, you don’t have to take anything
- it usually makes your periods lighter and shorter, and may stop them altogether after the first year
- about 20% of women stop having periods after 1 year, while 30% to 50% have no periods after 2 years
The contraceptive injection
Like the IUS, the contraceptive injection contains progesterone and is a long-acting type of contraception. Here’s what you need to know:
- each injection provides contraception for about 12 weeks
- research suggests it’s the form of continuous contraception that’s most likely to stop your periods
- more than half (55%) of women have no periods after 1 year of injections – and this rises to 68% after 2 years
- it may take up to a year for your fertility to return to normal after you stop using it
The contraceptive implant
Another long-acting contraceptive, the contraceptive implant slowly releases progesterone. Here’s what you need to know:
- a thin flexible rod is implanted under the skin on your arm by a doctor or nurse
- it provides contraception for 3 years
- while it can stop your periods altogether, you may just have lighter periods – and it can sometimes cause irregular or heavier periods
- research shows that about 2 in 10 women have no periods with the implant, while 3 in 10 have infrequent bleeding – but 2 in 10 have prolonged bleeding
Gonadotrophin-releasing hormone (GnRH) analogues
GnRH analogues are medications that suppress ovulation by stopping your ovaries from making oestrogen. Here’s what you need to know:
- they’re mainly used to treat pelvic pain and other conditions that are worsened by periods, such as endometriosis
- about 98% of women don’t ovulate or get periods after 8 weeks of taking them
- they create a temporary menopause, so side effects can include hot flushes, headaches, vaginal dryness and accelerated bone loss – which can increase your risk of weak bones (osteoporosis
When to see a doctor about skipping periods regularly
If you’re interested in regularly skipping your period, talk to your doctor. They’ll be able to help you assess the risks and benefits of each method, and which is safest for you to try.
For example, some treatments may have other side effects, which you may decide you’d rather avoid.
If you have a health condition that’s made worse by having periods (such as endometriosis), not having periods might be 1 of the possible treatments – although there may also be other solutions.
You should also see your doctor if you get heavy breakthrough bleeding while using 1 of the methods above, as this may be a symptom of an underlying problem, such as fibroids or a sexually transmitted infection (STI).
If you’re worried about any symptoms, you can try our Smart Symptom Checker to help you work out what to do next.
Your health questions answered
Does taking the pill continuously affect your fertility?
“Lots of people worry about this, but there’s no need – there’s no evidence that taking the combined pill long-term or back to back affects your fertility. Research shows that conception rates at 12 months after stopping the pill are similar to those of people who use non-hormonal forms of contraception.”
Is there a natural way to delay your period?
“No – the only way you can avoid having a period without taking medication is to get pregnant. Stress or illness may delay your period, but can’t be relied on as a method of controlling when your periods come.”
Can I still get pregnant if I intentionally delay my period?
“It depends what method you’re using to avoid having a period. Norethisterone only delays your period – it doesn’t offer any protection against pregnancy – but hormonal contraception is very effective at preventing pregnancy when used correctly. Even so, no method is 100% effective, and pregnancy does still occasionally happen. It’s worth remembering that it can be harder to know if you’re pregnant if you’re not having periods (a missed period is a common early sign). You may need to be more vigilant for other early signs of pregnancy, such as morning sickness and tiredness (fatigue).”







