Getting over long COVID
A lot of people who get COVID-19 have a mild illness and recover fully within a week or 2 of testing positive. But for some people, symptoms can last longer – for many weeks or even months – which is known as long COVID.
According to the latest figures, around 1.3 million people (2% of the UK population) report long COVID symptoms – meaning they currently have symptoms that have lasted for more than 4 weeks after they were infected. So if you’re struggling with lingering effects from COVID-19, you’re far from alone.
In fact, latest figures from a review of several international studies found that around 1 in 4 (26%) people who didn't end up in hospital with COVID-19 still had symptoms between 3 and 6 months later. This rose to more than half (57%) in patients who had been hospitalised with long COVID.
Recovering from symptoms as wide-ranging as extreme tiredness (fatigue), shortness of breath, concentration and memory issues (‘brain fog’), chest pain and anxiety can take time, and may be tough both physically and emotionally. But treatments are available and it’s important to seek help if you need it. (Read more about symptoms of long COVID.)
So read on to learn more about getting over long COVID, including when to see a doctor, and advice on treatments and self-care measures to support you on your road to recovery.
When to see a doctor about long COVID
No matter what your symptoms, you should see a doctor if they’re still affecting you more than 4 weeks since they started or you first tested positive for COVID-19.
Whether you go on to get long COVID doesn’t seem to be related to how ill you were when you first became infected with COVID-19 – some people with only mild symptoms to start with can develop longer-term problems. So don’t ignore lingering symptoms just because you had a mild COVID-19 infection originally.
You don’t have to deal with your symptoms alone. Your doctor will be able to offer support, give advice about self-management techniques and ways to track your progress, or prescribe medication if necessary.
If your symptoms are having a big effect on your life, they may:
- organise tests depending on your symptoms, such as blood tests or a chest X-ray
- refer you to a specialist for a particular symptom
- refer you to a long COVID clinic – this will have a team of different specialists, such as physiotherapists, occupational therapists and psychologists, who can help with various symptoms
How long does long COVID last?
COVID-19 is an area of constantly emerging research, and at present we don’t know exactly how long the symptoms of long COVID can last. What the latest science shows is:
- some people still have symptoms after getting COVID-19 in the first wave of infections in 2020
- for most people, symptoms gradually improve with time, although exactly how long this can take isn’t yet known
- even if you still have symptoms after 4 weeks, there’s a good chance that they will have improved or gone by 8 or 12 weeks. For example, recent data showed 13% of people still had symptoms after 4 weeks, but only 4.5% had symptoms after 8 weeks, and even fewer (2.3%) had symptoms lasting longer than 12 weeks
Is there a treatment for long COVID?
Unfortunately, there’s no specific ‘cure-all’ medication to help speed up recovery from all the symptoms of long COVID. But, as with other post-viral illnesses, help and treatments are available for specific symptoms. And experts are learning more about how to manage long COVID all the time.
Here’s how you can manage some of the more common long COVID symptoms, including breathlessness, fatigue, brain fog and low mood.

Coping with long COVID breathlessness
Shortness of breath is a common symptom of both COVID-19 and long COVID. Feeling out of breath may happen after you climb stairs or go for a walk, for example.
You should notice your breathing improving more over time, as you recover from the virus and start to regain your strength.
5 ways you can ease long COVID breathlessness
1. Practise controlled breathing. This can help you to relax and control your breathing:
- start by sitting in a supported, comfortable position
- place 1 hand on your chest and the other on your tummy
- shut your eyes and focus on your breathing
- slowly breathe in through your nose (or mouth if you can’t), then out through your mouth – you should feel the hand on your tummy move more than the hand on your chest as you breathe
- try to use as little effort as possible and make your breaths slow and smooth
2. Learn paced breathing. This is useful for activities that might make you breathless, such as climbing the stairs:
- think about breaking the activity down into smaller parts (eg stopping halfway) to make it easier to carry out without getting tired or breathless
- breathe in before you make the effort of the activity – before you climb up a step
- breathe out while making the effort – climbing up a step
- breathing in through your nose and out through your mouth may also be useful
3. Try positions that can help ease breathlessness. These include:
- lying on your stomach
- lying on your side with your knees slightly bent and your head and neck supported by pillows
- sitting at a table and leaning forward from your waist, with your head and neck resting on pillows
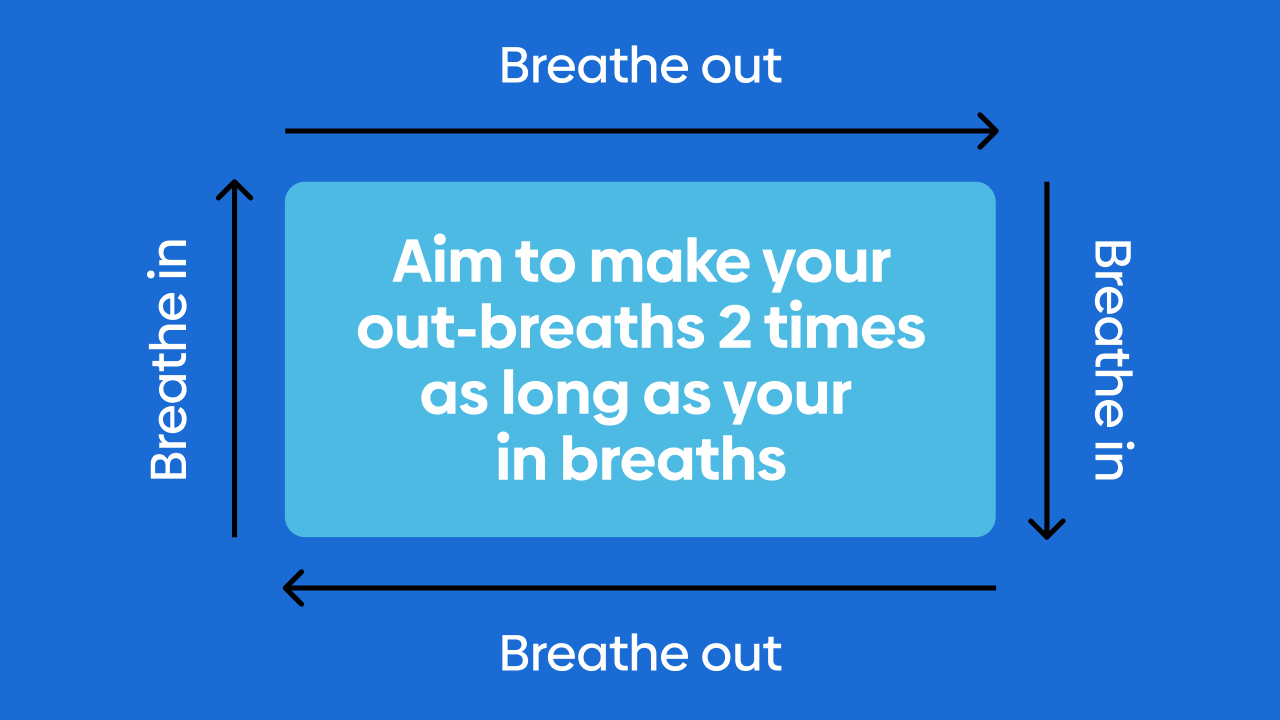
4. Breathe a rectangle. Look for a rectangle shape, such as a door or a window frame. Then follow the sides of the rectangle with your eyes as you breathe in and out. You should gradually slow down the speed so that your eyes move round the rectangle, pausing at each corner.
5. Wipe a cold flannel over your nose and upper cheeks. Cooling your face around your nose can help to reduce feelings of breathlessness.
When to see a doctor about long COVID breathlessness
If the exercises above don’t bring relief, see your doctor for advice, because:
- they may be able to refer you to a respiratory physiotherapist who specialises in lung conditions, who can help get you moving and teach you muscle strengthening exercises to help ease your breathing symptoms
- breathlessness can sometimes be a sign of severe COVID-19 and some of the complications that it can cause, such as blood clots
- being short of breath can also be a symptom of other conditions, including heart and lung problems or anxiety
If you have unusual breathlessness, especially when moving, or your breathing gets worse suddenly, seek urgent medical help.
Treatment for long COVID fatigue and muscle pain
Fatigue is common after viral infections and it’s one of the most common symptoms of long COVID. You can feel very tired despite resting or sleeping, or after only minimal exertion, to the point where you find it difficult to do normal day-to-day activities. Fatigue after long COVID is also closely linked to muscle aches and pains.
Long COVID fatigue is thought to be similar to the symptoms of other post-viral fatigue syndromes and chronic fatigue syndrome (CFS), so some of the treatments are similar.
5 ways to manage fatigue and muscle pain
1. Try this free online course by the Advanced Wellbeing Research Centre at Sheffield Hallam University, which can teach you about energy management – getting the right balance between rest and activity – during your recovery.
2. Plan ahead for each day or week, prioritising, spreading out activities and building in rest periods so you have time to recharge. Don’t compare yourself with others, or with what you used to do in the past. Pacing yourself will help you avoid overdoing things, which could make your symptoms worse.
3. Practise relaxation techniques, such as meditation, yoga or tai chi, and make time for other activities that help you chill out. This can help with fatigue and pain by reducing stress and promoting good sleep habits. Read about other activities for managing stress.
4. Use tips to improve the quality of your sleep, if you’re struggling with insomnia and it’s affecting your energy levels. If these don’t work, see your doctor. They may be able to prescribe medicines to help in the short term or refer you for therapy for sleep problems, such as cognitive behavioural therapy (CBT). Sleeping well can also help to reduce pain symptoms.
5. Exercise to regain muscle strength and endurance – but taking things slowly. With long COVID, it’s common for symptoms such as fatigue and muscle pain to get worse after exercise – this is known as post-exertional malaise (PEM). If you get PEM, it’s best to avoid activities that cause it as much as possible. For example, if you feel exhausted after doing a supermarket shop, try ordering online instead. You may need to build up to exercise very gradually, guided by how you feel.
Read more self-help tips to fight fatigue.

When to see a doctor about long COVID fatigue
You should see a doctor if your fatigue is getting worse rather than better, it doesn’t get any better over several weeks, or you also have other symptoms. They can check for any underlying conditions that might be causing it.
Coping with long COVID brain fog
Problems with thinking, concentration and memory – often known as ‘brain fog’ – are among the most commonly reported long COVID symptoms.
You may find it exhausting trying to deal with things that you previously found easy, have problems concentrating or finding the right words, or struggle with planning and organising tasks.
Brain fog can feel frustrating and worrying, but there are things you can do to help yourself. It’s also important to recognise why you’re struggling, and talk to your family and possibly your employer about it, so you can get their understanding and support.

6 tips for dealing with long COVID brain fog
1. Create an easy-to-follow daily routine to reduce the number of decisions you have to make each day. Decide what’s important to you and make a simple schedule. Doing the same things every day will mean you can eventually do them without thinking.
2. Set realistic goals to increase your motivation. To start with, think small: something such as reading a book for 10 minutes a day. When you achieve a goal, celebrate with a reward, such as a hot drink or your favourite TV programme.
3. Use memory aids – such as keeping a diary, putting sticky notes around the house or setting reminders on your phone. You can also use your phone to record or photograph things you need to remember.
4. Find a quiet time and place to deal with more complicated tasks, so you won’t be interrupted or distracted. You could try looking at music streaming sites for playlists that can help you focus.
5. Try brain exercises, such as puzzles or word and number games. Start with simple challenges and build up to more difficult tasks as you notice yourself improving. Trying a new hobby or just reading a book can also help stimulate your mind.
6. Ask friends and family for support. Explain what you’re going through and say you’d appreciate help with shopping or babysitting, or even just some time spent playing a board game to help you sharpen up.
When to see a doctor about long COVID brain fog
Talk to your doctor if your thinking and memory problems don’t improve over time, they’re quickly getting worse, or they’re severely affecting your day-to-day life.
Your doctor may suggest some tests, or refer you to an occupational therapist or psychologist for specialist help.

Treatment for long COVID low mood and depression
Low mood is another common symptom of long COVID. It’s not surprising that being ill can affect you emotionally, and it may take a while to get over what you’ve been through.
With some cases of low mood, you may be able to manage your symptoms with self-help measures, such as the suggestions below.
4 self-help measures to improve long COVID low mood
1. Take good care of yourself by eating a healthy, balanced diet, sticking to a sleep routine, taking regular exercise and avoiding drinking too much alcohol. It might be a good time to change some habits, too, such as quitting smoking if you smoke, or learn some meditation techniques.
2. Keep a recovery journal. By tracking your symptoms and feelings, you can see the progress you’re making. Writing down your feelings can also help you work through them and ‘step back’ from unhelpful thoughts.
3. Stay in touch with friends and family. It’s important not to isolate yourself, particularly if you’re feeling low. Feeling connected can help improve your mood.
4. Be kind to yourself. Any illness takes time to recover from, whether it’s physical or mental. So don’t expect too much of yourself, or get annoyed if you’re not able to do everything you feel you should be doing.
Read more about self-care for depression.
When to see your doctor about low mood and depression
If your negative feelings don’t go away after a few weeks, or they’re stopping you from doing normal activities, you should see a doctor. They may refer you for talking therapy (such as CBT) or prescribe antidepressants.
Always seek emergency medical help if you feel suicidal.
Read more about low mood and depression.
What helps long COVID anxiety symptoms?
Being ill with COVID-19 can be a frightening experience, especially if you have to go to hospital or get medical treatment. So it’s completely normal if you feel fearful and anxious afterwards.
Self-help tips for helping with symptoms of anxiety include:
- making a ‘balancing thinking’ chart – divide a page into 2 columns and write your unhelpful, anxious thoughts in 1 column and a more helpful, rational version in the other
- setting aside ‘worry time’ – scheduling a specific time in each day when you can think anxious thoughts can help you ‘switch off’ your anxiety at other times
- keeping busy – distract yourself from feelings of anxiety with activities you enjoy, such as chatting to friends, walking the dog or cooking a meal
- learning relaxation techniques – such as visualisation, when you picture a safe place, or mindfulness meditation, which helps you concentrate on living in the moment, rather than worrying about the past or future
When to see a doctor about long COVID anxiety symptoms
If your anxiety is severe and doesn't go away, talk to your doctor, who may be able to discuss medication or refer you to a psychologist or for therapy, such as CBT.
Find more information about managing anxiety.
Treatment for long COVID chest pain and heart palpitations
Some people with long COVID have reported chest pain and/or heart palpitations – where your heart beat suddenly becomes more noticeable.
This isn’t something you should ignore, so see a doctor about any new type of chest pain or palpitations to rule out anything serious, such as heart or lung conditions.
If you suddenly get bad chest pain, it lasts more than 15 minutes, or you have other symptoms such as nausea, sweating and shortness of breath, call for emergency medical attention, as these can be signs of a heart attack.
Other causes of chest pain that may be related to long COVID
-
muscular chest pain – this type of pain can be felt in a specific area on your chest, or you may get a more widespread muscle soreness called myalgia. It often happens during viral illnesses such as COVID-19, as it can be caused by straining during coughing, for example. Sometimes, the pain can last during recovery. It’ll usually go away after rest and avoiding activities that worsen the pain, and you can treat it with heat or ice packs and simple painkillers such as paracetamol or ibuprofen (speak to a pharmacist for advice on how to take these safely)
-
pleuritic chest pain – pain that is sharp and worse on breathing in can be a symptom of inflammation of the lining of the lungs (pleurisy) or heart (pericarditis). These can usually be treated with painkillers such as paracetamol and anti-inflammatory medication. But this sort of pain can also occasionally be a sign of a more serious condition, such as pulmonary embolism. See your doctor if you have pain that’s worse when you breathe in, and get urgent medical help if it’s severe, comes on suddenly or you also have trouble breathing or you’re coughing up blood
Postural orthostatic tachycardia syndrome (PoTS) and long COVID
Some people with long COVID get symptoms that are similar to a condition called postural orthostatic tachycardia syndrome (PoTS). This can cause dizziness when you get up and heart palpitations, and can be triggered by an infection.
Once diagnosed, PoTS can be managed with diet, exercise and medication, so see your doctor if you think you have symptoms. Read more about how PoTS is treated.
Places to go for support with long COVID
Of course, your doctor should be the first place you go for help with treatments and referrals to specialists for long COVID symptoms. But there are also other resources, support groups and online forums you can try:
-
the NHS website Your COVID Recovery has lots of information, while the Your COVID Recovery programme is an app your doctor can refer you to
-
covid:aid is a UK national charity offering information, where you can also connect with other people affected by long COVID
-
Long COVID Support is a patient group offering support and information about managing your condition
-
HealthUnlocked is an online forum where you can share experiences and tips for treating and living with long COVID
One to watch
A drug to treat fatigue in people with long COVID is currently being clinically tested. Called AXA1125, it targets your mitochondria – the ‘power plants’ of your body’s cells, which make energy. The theory is that mitochondria may not work properly in people with long COVID.
The trial’s lead researcher, Dr Betty Raman, said: “Long COVID is having a truly devastating impact on countless people around the world, leaving many with a sense of hopelessness. It is widely recognised that mitochondrial dysfunction may contribute to the profound fatigue associated with this condition. With no approved long COVID therapies, the need for continued innovation is urgent. I am pleased to be leading an investigation of AXA1125 to understand its potential to restore cellular energetics and address patients’ needs.”
Your health questions answered
Can long COVID affect your periods?
Answered by: The Healthily medical team
“It's common for your periods to be affected when you’re unwell, as stress and illness can disrupt the brain hormones that communicate with your ovaries. But this shouldn’t last longer than a few menstrual cycles. Some people have reported changes to their cycle after COVID-19 and there have been a small number of studies. Based on the limited evidence we have so far, it seems that any changes are only temporary, and don’t appear to affect fertility in the long term. A review of 12 studies on the effects of COVID-19 on the menstrual cycle found evidence of changes (mainly longer cycles and lighter periods), due either to stress and behaviour changes or the illness itself, but said further research was needed. If your periods have stopped for longer than 3 months or you’re bleeding when you’re not on your period, you should speak to your doctor.”
Are migraines a symptom of long COVID?
Answered by: The Healthily medical team
“Viral infections can make existing migraine headaches worse – they may last longer than usual and you may get them more frequently. Long COVID headaches may also be more frequent if you already have a history of headaches. Try to avoid your migraine triggers, which may include skipping meals, stress or lack of sleep, and practise relaxation techniques. You can treat your symptoms with painkillers or migraine medication. Read more about migraine treatment.”
Are there any vitamins or supplements that help with long COVID?
Answered by: The Healthily medical team
“At present there aren’t any particular vitamins or supplements recommended for long COVID. However, it's a new condition that we’re learning more about all the time, so there may be certain nutrients recommended in the future. If you don't think you’re getting all the nutrients you need from your diet, a multivitamin may be helpful. Depending on your symptoms, your doctor may also want to check your levels of certain vitamins or minerals, such as iron, and may advise a supplement if blood tests show a deficiency.”
Is there any evidence that the Omicron variant causes different long COVID symptoms?
Answered by: The Healthily medical team
“Omicron was first reported at the end of November 2021, so those who were first infected may be still in the process of recovery. This means we probably won't have answers about what long COVID symptoms the variant causes for some time. What we learn about how Omicron affects long COVID might also be changed by the vaccine and its impact on long COVID.”







