Periods are part of life for millions of women throughout the world, and more and more people now talk about them openly. However, if you have worries or questions about blood clots, flooding, or how your period blood should smell, it can feel like these sorts of topics are still off limits for discussion.
But how will you know what’s normal and what’s not if you can’t talk about it? Healthily is on a mission to help women get the healthcare they deserve – and this starts with frank and honest answers to these sorts of questions.
Periods might be a normal part of life, but that doesn’t mean they’re easy. On the days when you bleed from your vagina, cramps can really hurt, while heavy blood loss can leave you feeling exhausted. Not to mention period symptoms such as bloating, backache and mood swings, or broken sleep from getting up at night to change towels or tampons.
According to the UK charity Women’s Health Concern, although 1 in 3 women describe their periods as heavy, only 1 in 20 see a doctor about it. And in a 2018 survey by children’s charity Plan International UK, nearly 80% of girls and young women said they’d had period symptoms that worried them, but hadn’t seen a doctor. More than a quarter stated that they didn’t get medical advice because they were too embarrassed.
But this stigma means you may miss out on things that can help you, such as self-care tips for period pain, or medication to help with heavy bleeding. Or, even worse, symptoms of underlying medical conditions that need treatment could go unnoticed.
So read on to get the Healthily lowdown on periods, including how to sort any problems and when you should see a doctor. You can also use our Smart Symptom Checker to help you decide the best next steps for you.
What are periods and the menstrual cycle?
Your menstrual cycle is the monthly process your body goes through to prepare for a possible pregnancy.
During each cycle, you release an egg (ovulation) and the lining of your womb (uterus) gets thicker to hold the egg after it’s been fertilised by sperm. But if the egg isn’t fertilised, the thickened womb lining isn’t needed, and leaves your body through your vagina as your period.
Your menstrual cycle is controlled by the hormones oestrogen and progesterone:
- after your period finishes, your levels of oestrogen increase, which causes 1 of your ovaries to release a mature egg
- after you ovulate, progesterone makes the lining of your womb thicker to prepare it for the fertilised egg
- if the egg isn’t fertilised, your levels of oestrogen and progesterone fall, and this triggers your period
Read more about what happens during the menstrual cycle.
How often do you get your period?
Here’s what you need to know:
- your menstrual cycle and periods start when you go through puberty, which usually happens when you’re about 12 years old. Aside from during any pregnancies, your periods will then continue until you reach the menopause
- each menstrual cycle runs from the first day of your period to the day before your next period. An average cycle lasts 28 days, but can vary between 21 and 35 days
- it’s common to have irregular periods for the first 2 years after they start. This is usually nothing to worry about, and your cycle will eventually settle down into a regular pattern
- missing a period can be an early sign of pregnancy. If you think you could be pregnant, do a test as soon as possible – read about how to use a pregnancy test
- various other things can cause irregular or absent periods, including stress, hormonal birth control (contraception) and medical conditions (read more about this below)
What are the signs that you’re getting your period?
After years of having periods, most of us are familiar with the clues from our body that tell us it’s on its way (although not everyone gets them).
Known collectively as premenstrual syndrome (PMS), these symptoms can start up to 2 weeks before your period is due, and commonly include:
- breast tenderness
- bloating or tummy pain
- headaches
- tiredness
- feeling sick (nausea)
- loose poos (diarrhoea)
- lower back pain
- breakouts of spots (acne)
- feeling upset, anxious or depressed
- food cravings
It’s also common to get period pain, usually felt as muscle cramps in your lower tummy. This often happens at the start of your period, but some people also get it just before their period begins, or throughout their whole period.
Learning how to track your period and any related symptoms can help you predict when your period will start. You can use the Healthily self-care app to help you do this.

How long does each period last?
Periods can last between 3 and 8 days, with the average being 5 days. The flow of blood is usually heaviest on the first 2 days, then gets lighter, but this can also vary. The important thing is getting to know what’s normal for you – and then you’ll know if anything changes.
How much do you bleed?
We keep saying this, but it really does vary. However, blood loss of 30ml to 40ml (8 to 11 teaspoons) is considered to be average, while the majority of women (9 out of 10) lose less than 80ml (16 teaspoons) of blood during a period.
How much blood you lose during a period can also vary at different stages of your life. For example, heavy bleeding tends to increase with age, peaking in women aged 30 to 49.
Remember that period bleeding isn’t like cutting your finger – it doesn’t usually just go on and on. The flow is regulated by your hormones, which control the shedding of your womb lining. So once this process is finished, the bleeding usually stops.

How to tell if your bleeding is heavy
If you lose more than 80ml of blood, and/or your period lasts more than 7 days, your periods are considered to be excessively heavy – known as menorrhagia.
So how can you tell if that’s you? Experts say heavy bleeding is when:
- you need to change your towel or tampon (sanitary protection) every 1 to 2 hours
- you see clots of blood that are bigger than 2.5cm (see below)
- you need to use a towel and a tampon at the same time
- blood floods through your clothes
- you see a doctor because you feel that your periods are very heavy
Having heavy periods doesn’t necessarily mean there’s a problem, but it does need to be investigated. It may turn out that heavy bleeding may just be normal for you, and in many cases, no underlying cause is found.
But there are some conditions that are linked to heavy periods, including conditions that affect your hormones, ovaries or womb (see below for more information).
Are blood clots a normal part of a period ?
It may feel scary if you see a blood clot on your towel or tampon. But as long as they’re not bigger than 2.5cm (about the size of an average cherry), it’s normal.
Clots are less worrying once you know that they’re formed by your body to stop you losing too much blood from blood vessels in the lining of your womb – so actually, they’re a safety mechanism.
However, if you’re frequently seeing clots that are bigger than 2.5cm, you should see a doctor, as they could be a sign of an underlying medical condition.
Possible causes of abnormal blood clots include:
- fibroids – non-cancerous growths in and around your womb
- uterine polyps – mostly non-cancerous (benign) growths on the lining of your womb
- bleeding disorders such as Von Willebrand disease (VWD)
- thyroid problems (hypothyroidism)
- cervical cancer or cancer of the womb
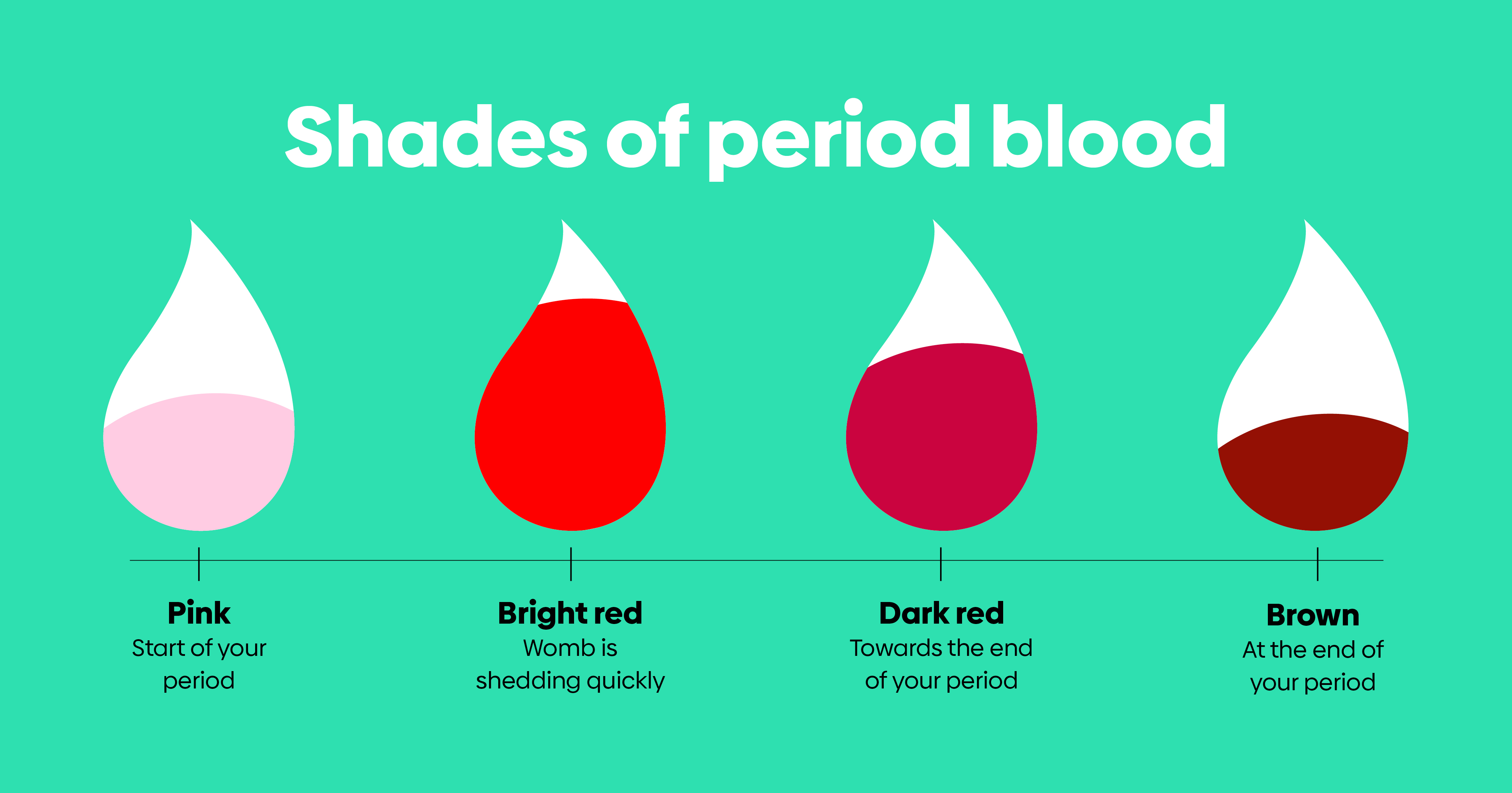
What colour should my blood be ?
The colour of your period blood isn’t usually anything to worry about, and it will vary at different stages of your period. On the days when your flow is heaviest, the blood will be red, while on lighter days, it can be pink, brown or black.
Here's what you need to know:
- pink period blood – usually comes at the start of your period, and it’s pink because it’s mixed with vaginal mucus
- bright red period blood – comes when the lining of your womb is shed quickly, as your womb squeezes (contracts) to push it out
- dark red period blood – usually comes towards the end of your period. Your womb doesn’t contract as fast at this stage, so the blood has more time to react with oxygen and gets darker
- brown period blood – usually comes towards the end of the period, when older blood mixes with vaginal mucus
Should my period blood smell?
It’s normal for period blood to smell. It smells different from the blood that flows if you cut your finger, because it’s been inside your vagina and mixed with the friendly bacteria that help keep your vagina healthy.
As with most things to do with your periods, you’ll get to know what smells normal for you. If the smell changes, or is suddenly really unpleasant, you should check that you haven’t forgotten to remove a tampon, or speak to a doctor in case it’s a sign of a vaginal infection.
You can keep yourself fresh during your period by:
- washing or showering regularly – there’s no need for vaginal washes, you should just use water to clean your genitals
- frequently changing your period products (tampon/towel/cup)
- always wearing clean underwear
Read more about hygiene during your period.

What does a normal period look like?
As you now know, there’s a wide range of menstrual cycle and period lengths, blood volume and colours, and lots of different types of periods are considered ‘normal’. What’s important is getting to know your own body and cycle, so you know what’s normal for you.
It’s also a good idea to be aware of the things that can affect your period, including various aspects of your lifestyle, your lifestage, certain medications and underlying medical conditions.
What can affect my ‘normal’ period?
Stress
Stress can affect when your periods come and how long they last for. You might find your cycle gets longer or shorter than normal, or your periods might stop altogether.
This is related to high levels of the stress hormone cortisol, which can disrupt the hormones that control your cycle. Read about techniques and tips for stress relief.
Jet lag
Travelling across time zones upsets your natural body clock (circadian rhythm), which controls your sleeping and waking pattern. It’s thought that this can also interfere with your hormone balance and disrupt your periods, although more research is needed.
Read more about jet lag symptoms, causes and treatment.
Smoking
Research shows that smokers are more likely to get painful periods. And if you’re a heavy smoker (at least 20 cigarettes a day), studies suggest this may disrupt your cycle and make it shorter.
Extreme weight loss or weight gain
Losing a lot of weight quickly – such as by dramatically restricting your calories – can stop your body from making the hormones needed for ovulation, so your periods can stop.
On the other hand, being very overweight (obese) can cause your body to produce too much oestrogen and affect the length of your cycle.
Over-exercising
Losing too much body fat by over-exercising can stop you from ovulating, and the stress of too much exercise can affect your period hormones.
Contraception
If you’re using hormonal contraception, such as the combined pill or an intrauterine system (IUS), you may find that your periods become lighter and shorter, or disappear completely. In fact, these are sometimes prescribed to help with very heavy periods (see below).
If you’re using an intrauterine device (IUD), on the other hand, your periods may get heavier and longer.
Pregnancy
Your periods will stop if you’re pregnant, and this usually continues after the birth if you’re exclusively breastfeeding.
Menopause
The menopause is when you stop ovulating and having periods, which usually happens between the ages of 45 and 55.
In the months and years leading up to this – known as the perimenopause – your periods can also change, due to hormonal fluctuations. They may become lighter or heavier, longer or shorter, and you may skip periods. Read more about perimenopause periods.
Medication
Some prescribed medications can affect your periods as a side effect, including:
- anticoagulant medicines – sometimes known as ‘blood thinners’, these can be prescribed to treat blood clots and prevent strokes, and can cause heavier periods. The most common type is warfarin
- some cancer medications – chemotherapy or hormone treatment for breast cancer can affect how your ovaries work and disrupt your periods. If this could be permanent, your doctor will discuss this with you before you start treatment, as well as any steps you can take to preserve your fertility
- medications for some of the medical conditions listed below
Medical conditions
Several underlying medical conditions can affect your periods, including:
- polycystic ovary syndrome (PCOS) – a common condition that affects how your ovaries work and can cause irregular periods
- premature ovarian failure – when your ovaries stop working normally before the age of 40, which can also cause irregular periods (read more about early menopause)
- pelvic inflammatory disease (PID) – this infection of the ovaries, fallopian tubes and womb can cause painful and heavy periods, as well as bleeding between periods and after sex
- fibroids – as mentioned above, these benign growths in and around the womb can cause large blood clots, as well as heavy or painful periods
- endometriosis – this is when tissue that’s similar to the lining the womb grows in other places, which can cause painful and heavy periods
How to look after your wellbeing during your period
Periods affect everyone differently. You might be lucky and not have any major symptoms, or you could get problems with every period – or you may just get issues from time to time.
If you do get period symptoms, they can have a big impact on your work and social life. Maybe you’ve cancelled a big night out because you’ve got your period, or called in sick with a ‘cold’, when it’s really terrible period pain that's had you doubled over?
Blood leaks can be a drag, too, ruining clothes or stopping you from feeling like running or going to the gym.
You may also struggle with PMS in the weeks running up to your period, and have to deal with mood swings, bloating, backache and acne.
If you have heavy periods, meanwhile, you may feel fatigued and washed out, and be at risk of getting iron deficiency anaemia due to blood loss.
So it’s important that you don’t just put up with period problems and let them carry on month after month. Start by trying these self-help tips to manage your symptoms, or ask your doctor for help to find solutions.

Self-care tips for managing your period
- track your cycle and symptoms – so you know when to expect your period and can tell your doctor what impact your periods are having on your everyday life. You can do this on the Healthily self-care app
- use a hot water bottle – putting a hot water bottle on your tummy is a popular way to help reduce period pain, and scientific studies have shown that it can be effective. Just wrap it in a cloth to avoid burning your skin
- have a warm bath – as with the hot water bottle, the heat can help ease pain, while having a bath can also help you relax
- give yourself a massage – gently massaging your lower tummy with light, circular movements can help ease painful cramping
- do some gentle exercise – you may just feel like curling up on the sofa, but there’s evidence that exercise can improve period pain. And in a (unpublished) survey of more than 14,000 women by researchers from St Mary’s University, London, 78% said exercise reduced symptoms related to their cycle. Try something like swimming, yoga or a walk
- take painkillers – non steroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen and aspirin, can help with period pain. But they’re not suitable for everyone, so check with your doctor before you use them. You can also try paracetamol, but evidence shows that it may not work as well as NSAIDs
- quit smoking – if you smoke, giving up may help, as smoking is thought to increase your risk of painful periods
- stock up on period products – it’s a good idea to always have a stash at home, in your handbag or in your desk at work, so you’re prepared if your period starts unexpectedly. Read more about different types of period products
Read more tips for coping with period pain and try natural remedies for back pain during your period.
Stopping or skipping your period
It’s common to think that having periods is somehow ‘healthy’, and something every woman just has to put up with. But you can use medication to delay, control or stop your period.
If you want to skip a period because you’re going on holiday or have a big event coming up, you should talk to a doctor for advice about what treatment is right for you. But these are some of the options:
- norethisterone or medroxyprogesterone acetate – you may be able to take 1 of these medications for 3 to 4 days before your period is due. They need to be prescribed, so speak to your doctor or an online prescription service to see if either is suitable for you (not everyone can take norethisterone because it can increase your risk of blood clots)
- back-to-back combined pill – running several contraceptive pill packets together, so you have fewer (or no) breaks between pills, is another option for skipping or stopping periods. Not having periods while taking contraception won’t do you any harm
- IUS – using an IUS such as the Mirena coil may stop your periods completely, if this is what you’d prefer, although it doesn’t happen for everyone
Read more about delaying your periods.
What if I don’t have periods anyway?
If you’re not having periods or they’ve stopped, and you don’t know why, it’s important to see your doctor, so they can check what’s going on. Read about causes of and treatment for absent periods.

When to see a doctor about your periods
You should see your doctor if:
- you have very heavy periods that are causing discomfort or worry
- your periods are less than 21 days apart or more than 35 days apart
- your periods last longer than 7 days
- you don’t get a period for more than 3 months and you’re not sure why
- you get bad period pain or PMS that affects your daily life or mental health
- you notice bleeding between your periods
- you have pain or bleeding during or after sex
- you have any bleeding after the menopause
- you notice unusual bleeding from other parts of your body
- you’re losing weight without meaning to
- your tummy looks swollen or you can feel a lump
Depending on your symptoms, your doctor may offer advice, prescribe treatment (see below), or refer you to a specialist who can check for underlying medical conditions.
How to help your doctor to help you
When you go for your appointment, you can help your doctor by providing information about your family and medical history, and your symptoms and how they’re affecting you. This is why it can be helpful to use a diary or the Healthily self-care app to track your symptoms.
Your doctor may also ask about any other medication or treatment you’re having, including what contraception you’re using.
Medical treatment for period problems
How your period problems are treated will depend on your symptoms and what’s causing them. Treatments your doctor may recommend for bleeding problems or PMS include:
- combined pill – this can make your periods lighter, more regular and less painful, and may also reduce symptoms of PMS
- progestogen-only pill (POP, mini pill) – this can also make your periods lighter, or stop them altogether, although it may cause irregular or more frequent bleeding. It can help with PMS symptoms and painful periods, too
- IUS – this can make your periods much lighter or stop them completely, so can be used to help with very heavy or painful periods
- tranexamic acid – this helps your blood to clot, so reduces bleeding and can be used to treat heavy periods. It’s usually prescribed as a tablet that you take for a few days every month
Read more about treatment for heavy periods, irregular periods and PMS.
If an underlying medical condition is causing your period problems, you’ll be offered treatment for this. You may be referred to a specialist in female reproductive health (gynaecologist) or hormone conditions (endocrinologist).
Treatment for underlying conditions may include medication or surgery. Read more about treatment for PCOS, PID, fibroids and endometriosis.
Your health questions answered
Is it unhealthy if you don’t bleed every month?
Answered by: The Healthily Medical Team
“Some people worry that it’s ‘unhealthy’ not to have a period, and think that blood ‘builds up’. But in many cases, not having periods won’t do you any harm. If you’re pregnant, breastfeeding or taking hormonal contraception, for example, blood doesn’t build up and your womb lining stays thin. And there’s nothing wrong with using contraception to miss some or all of your periods. Our ancestors had far fewer periods, as they were nearly always pregnant or breastfeeding and often died at a younger age – so you could argue that it’s unnatural to have so many periods. However, if there’s another reason for you not having a bleed every month – such as PCOS – your womb lining can build up, and it’s recommended that you have at least 3 bleeds a year. So it’s important to see a doctor if you’re not having regular periods, to check for underlying causes.”
Can you have a period twice a month?
Answered by: The Healthily Medical Team
“While it could just be a very short menstrual cycle, you should see a doctor if you’re bleeding twice in a month. This is because it could mean you’re bleeding between periods – medically known as ‘intermenstrual bleeding’. Your doctor will probably examine you and may suggest some tests, such as a smear test, sexual health screen, blood tests and possibly an ultrasound scan. Read more about when to see a doctor about irregular periods.”
Can you have a period if you’re pregnant?
Answered by: The Healthily Medical Team
“In the early weeks of pregnancy, you may notice some light bleeding or spotting. Known as ‘implantation bleeding’, this is caused by the fertilised egg embedding itself in the lining of your womb, and is usually nothing to worry about. But bleeding in pregnancy can also be a sign of miscarriage or an ectopic pregnancy, so it’s important to see your doctor to get it checked. (An ectopic pregnancy can be life-threatening, so if you have tummy pain as well as bleeding, get emergency medical help.) Although you should always get it checked, occasional bleeding in pregnancy is often nothing to worry about. For example, you may have hormone-related bleeding at 4 to 8 weeks, or around the time your period would have been due. This will normally stop at around 13 weeks, once the placenta is properly developed.”







